The Practice of Catheter Cryoablation for Cardiac Arrhythmias
Edited by Ngai-Yin Chan


Cases
Case 2.1. Standard cryoablation for atrioventricular nodal reentrant tachycardia
The patient is a 10-year-old male with a history of supraventricular tachycardia. He was having a snowball fight when he noticed an acute onset of rapid heart rate. He felt chest tightness, palpitations, shortness of breath, and dizziness. He was taken to an emergency room and found to be in a narrow complex tachycardia at 220 beats per minute (bpm). Vagal maneuvers were attempted but unsuccessful. He required two doses of adenosine to convert to a sinus rhythm. This episode lasted 30 min. He likely has had a few other episodes, all around exercise. He denies syncope and seizures. He has normal exercise tolerance. He had a normal echocardiogram. See Figures 1 and 2.
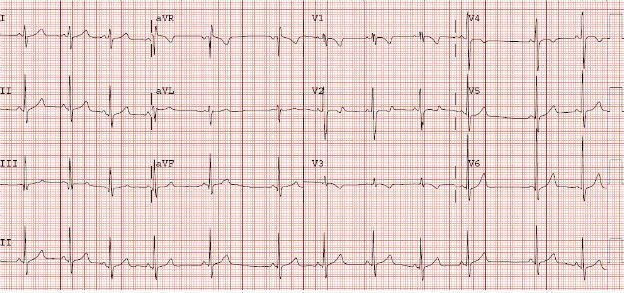
Figure 1. Baseline 12-lead electrocardiogram (ECG) shows normal sinus rhythm and no evidence of preexcitation.
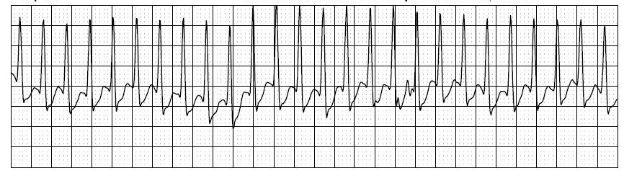
Figure 2. Event monitor tracing in tachycardia shows a regular narrow complex tachycardia with no evidence of retrograde P-waves.
A discussion with the patient and his family involved discussing treatment options of clinical monitoring, antiarrhythmic medications, or an invasive electrophysiology study and ablation procedure. After discussion of the risks and benefits, the family chose to proceed to ablation.
Invasive Electrophysiology Study - At the electrophysiology study, the findings showed evidence of an AH jump with A1A2 pacing as well as evidence of sustained slow pathway conduction with atrial overdrive pacing. There was easily and reproducibly inducible typical atrioventricular nodal reentrant tachycardia (AVNRT) with pacing around the block cycle length. Retrograde conduction was central and decremental, and an accessory pathway was ruled out.
Cryoablation - The HRA catheter was removed, and a 6 mm tip cryoablation catheter was advanced to the right atrium. It was placed at the lower one-third of the triangle of Koch, with an almost equal "A" and "V" signal. Cryoablation was conducted with a series of lesions in a linear fashion. A total of four lesions were placed. Post cryoablation, there was no longer sustained slow pathway conduction and no AH jump. There was no further inducible tachycardia. See Figure 3.
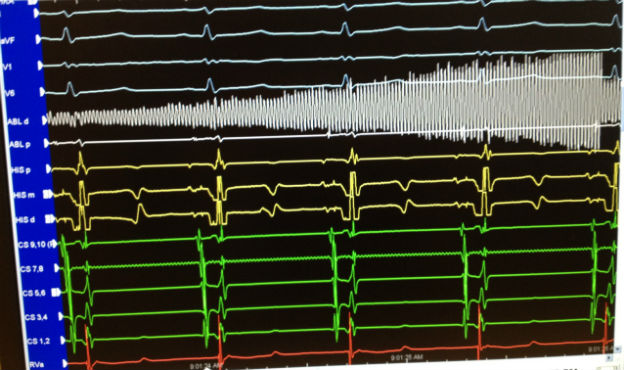
Figure 3. Intracardiac tracing during cryoablation for typical atrioventricular nodal reentrant tachycardia. Cryoablation was applied in normal sinus rhythm,and the atrioventricular nodal conduction was continually monitored.
-
1. Why was cryoablation utilized (instead of radiofrequency catheter ablation)?
-
2. How does cryoablation for AVNRT compare with RFCA in terms of recurrence rates?