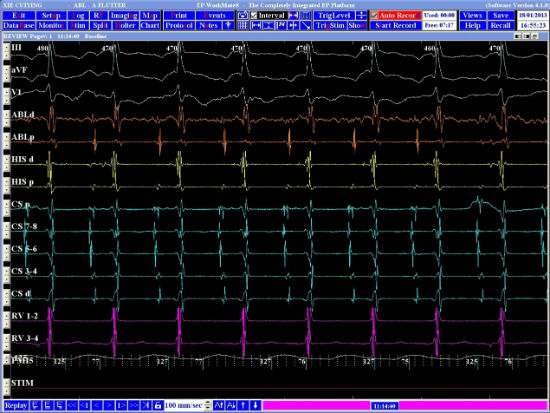
A 21-year-old woman who has a history of prolapsed mitral valve and trivial mitral regurgitation since her teenage years presented with paroxysmal fast palpitations. Electrocardiogram revealed long RP tachycardia. The patient was in incessant supraventricular tachycardia (SVT) during the cardiac electrophysiology study (Figure 1).
-
1. What is the most likely mechanism for the SVT – atypical atrioventricular nodal reentrant tachycardia (AVNRT), permanent junctional reciprocating tachycardia (PJRT), or focal atrial tachycardia?
Show Answer
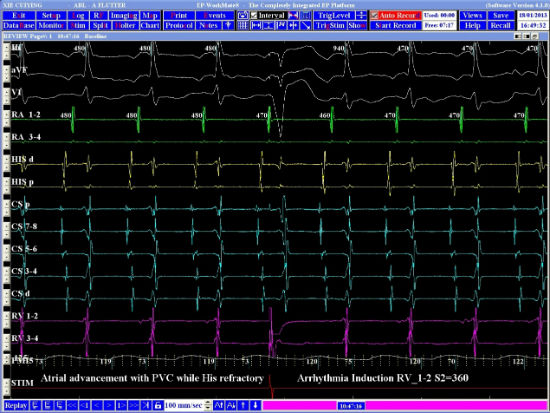
Correct answer: It is most likely PJRT. Differential diagnoses of long RP tachycardia include atypical AVNRT, PJRT, and atrial tachycardia. Intracardiac electrograms during SVT revealed earliest atrial activation at the ostium of the coronary sinus. Reproducibly, a premature ventricular contraction delivered when the His bundle was refractory advanced the next atrial activation. This phenomenon was diagnostic of the presence of an accessory pathway. Coupled with the clinical information of an incessant long RP tachycardia, the most likely diagnosis was PJRT. (Also see Video Clip 8.1 for catheter cryoablation in a case of atrial flutter.)
-
2. Radiofrequency ablation with a 4 mm tip catheter was attempted at the right and left posteroseptal regions without terminating the tachycardia. What would be your subsequent approach – catheter cryoablation inside the coronary sinus, radiofrequency ablation inside the coronary sinus, or saline-irrigated radiofrequency ablation at the right or left posteroseptal region?
Show Answer
Correct answer: Catheter cryoablation inside the coronary sinus. Failure of endocardial radiofrequency ablation in the posteroseptal area suggests epicardial location of the accessory pathway. Increasing the depth of lesion endocardially by saline-irrigated radiofrequency ablation may not be the best approach. Both radiofrequency and cryoablation within the coronary sinus are acceptable strategies. However, radiofrequency ablation inside the coronary sinus may be more risky in terms of collateral damage like coronary artery damage.
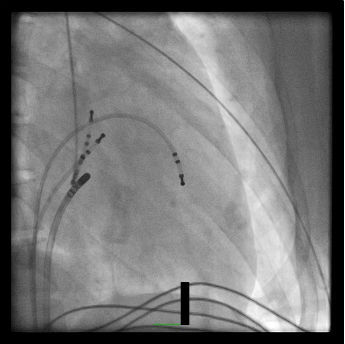
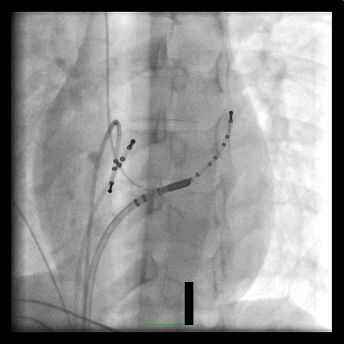
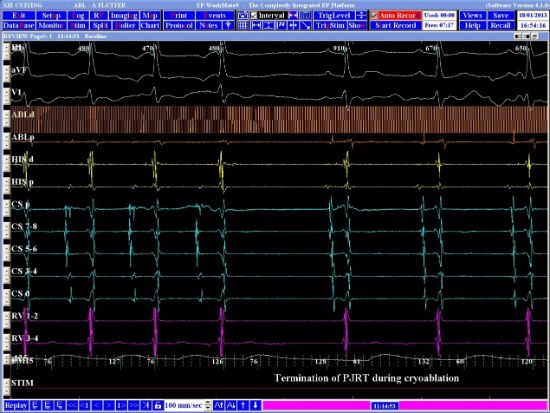
Cryoablation with an 8 mm tip catheter was positioned inside the proximal part of coronary sinus (Figures 2A and 2B). Atrial activation was earliest at the ablation catheter (Figure 2C). Termination of PJRT was observed very soon after initiation of cryoablation (Figure 2D).
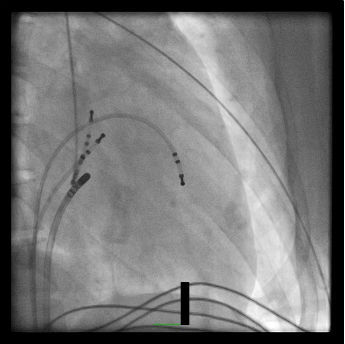
Figure 2A
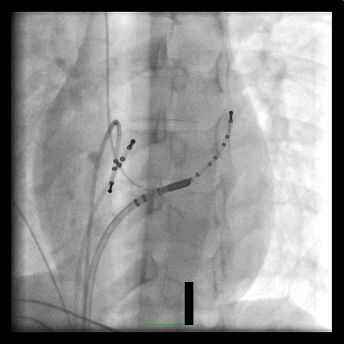
Figure 2B
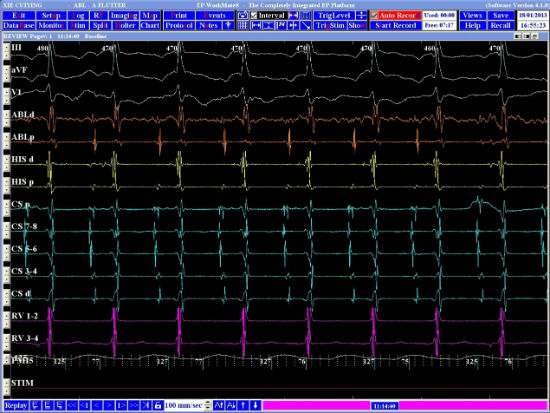
Figure 2C
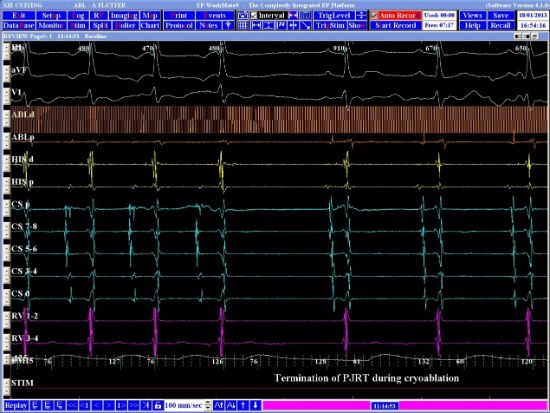
Figure 2D